
Perpetuating factors, such as worry about not being able to sleep, rumination, and behaviors such as waiting long hours in bed to sleep, irregular sleep schedules, naps, and activities in bed other than sleeping, cause acute insomnia to become chronic. Precipitating factors for acute insomnia are stressors that negatively affect sleep, such as illness, the burden of work or school, and interpersonal conflict. Predisposing factors, including hyperarousal traits and a family history of insomnia, increase vulnerability to insomnia. The 3P model describes the mechanism of chronic insomnia on the basis of predisposing factors, precipitating circumstances, and perpetuating factors. Spielman’s 3P model, which best conceptualizes the mechanism by which insomnia becomes chronic, was published in 1986. This helps establish a consistent sleep rhythm and 6) do not take naps. Do not lie in bed for more than 10 minutes without falling asleep 4) if you still cannot sleep, repeat the previous steps 5) wake up at the same time each morning, no matter how much you slept. Stay up as long as you want and go back to your bedroom. Do not read, watch television, eat, or worry in bed 3) if you cannot sleep, get up and go to another room. Stimulus control therapy consists of the following guidelines: 1) sleep only when you are sleepy 2) do not use your bed for anything other than sleep and sexual activity. Stimulus control therapy develops a coherent sleep-wake pattern by reinforcing beds and bedrooms with conditioned sleep stimuli and dissociating conditioned stimuli with behaviors that are incompatible with sleep.
These stimuli, which include bedroom and bed environments, may illicit stressful and fearful feelings that reinforce the difficulty of falling asleep. Stimulus control therapy for insomnia is based on learning theory related to sleep, which is based on the assumptions that external or psychological factors that make it hard to fall asleep act as stimuli. In the 1970s, Bootzin’s stimulus control therapy for insomnia was introduced as the first non-pharmacological treatment specifically developed for insomnia. The first clinical study of insomnia treatment using relaxation therapy was published in the 1960s. In subjective reporting, muscle relaxation therapy reduces sleep onset latency and increases total sleep time. Progressive muscle relaxation therapy reduces muscle tension and stops racing thoughts that affect sleep. Progressive relaxation therapy was first developed by Jacobsen in the 1930s and is effective for insomnia patients. Muscle relaxation is the beginning of non-pharmacological insomnia treatment. Keywords: Insomnia, Sleep disorder, Cognitive behavioral therapy, Internet-based intervention INTRODUCTION INTRODUCTION This review will discuss the history of CBTi as a first-line treatment for insomnia, the current status and limitations of CBTi, the efficacy of dCBTi as an alternative, and the future of dCBTi in pioneering digital therapeutics.

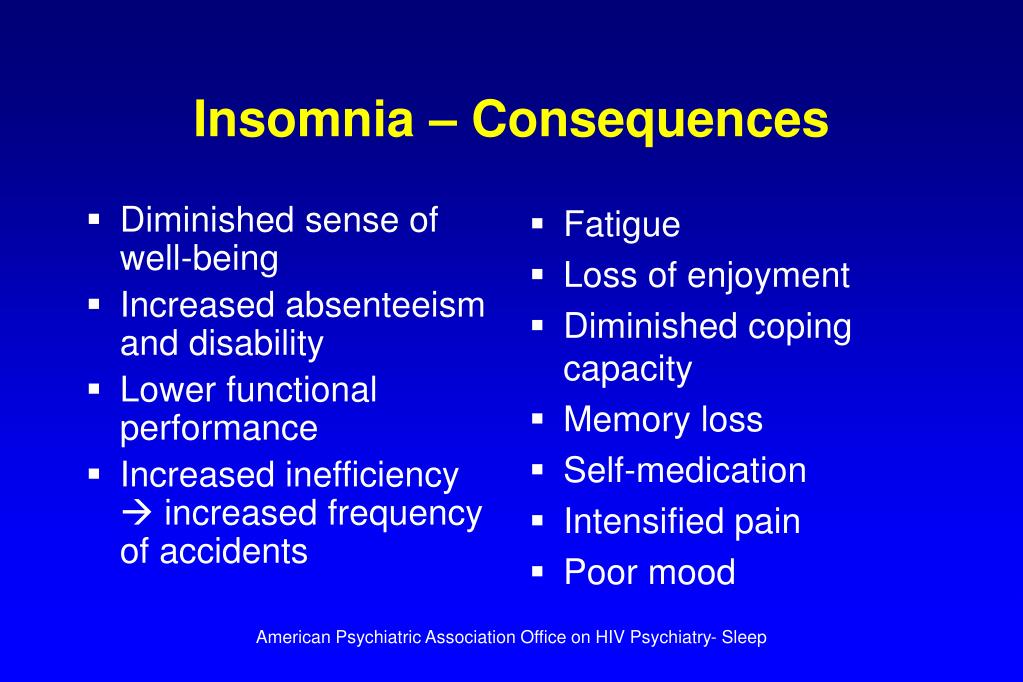
Recently, internet-delivered digital CBTi (dCBTi) has emerged as a potential answer for the growing demand and poor treatment accessibility. Despite considerable evidence of CBTi efficacy, accessibility and cost remain major barriers. Conventional CBTi is a multicomponent intervention program that includes: 1) a behavioral component made up of stimulus control therapy, sleep restriction therapy, and muscle relaxation 2) a cognitive component and 3) an educational component focused on sleep hygiene. The current first-line treatment recommended for insomnia is cognitive behavioral therapy for insomnia (CBTi). Therefore, the demand for insomnia treatment is high. Insomnia is highly prevalent, with a high relapse rate and a tendency to become chronic. By definition, insomnia must affect important areas of functioning and occur more than three nights per week for at least 3 months. Insomnia is a sleep disorder characterized by clinically significant distress caused by difficulty in initiating or maintaining sleep, or early-morning awakening.


 0 kommentar(er)
0 kommentar(er)
